
Diagnosing an invisible disorder
23 June 2021- Health & wellbeing
- Courage
- Ideas & info
Do you know the warning signs of PTSD?
Like a lot of health conditions, PTSD is often easier to manage when caught early. But recognising the mental scars of trauma can be tough. From obvious indicators such as flashbacks and nightmares, to more subtle red flags like mood changes and avoidance, a range of symptoms can indicate the onset of PTSD.
Withdrawal
According to Georgia, withdrawal is a classic warning sign of PTSD among military personnel.
“Quite a common one, particularly for veterans, is not wanting to go to shopping centres or do the shopping anymore, or go and watch the kids play sport, or go to any environment where there's a crowd of people – because that can leave somebody feeling quite vulnerable if they can't control their environment.”
Georgia explains that changes in a person’s routine can also reveal a lot about their mental state.
“It’s important to keep in mind that, as human beings, we're quite predictable in what we do.
“For me, I get up, I get in my car, and I go to work every day. I have lunch at the same time each day. On the weekends I might go for coffee and socialise a bit with my girlfriends.
“But if I was experiencing PTSD, somebody might notice that I'm actually not doing those things as often as I used to.”
Mood changes
Experiencing or witnessing a traumatic event can leave your brain stuck in fight, flight or freeze mode, even when the danger has long since passed. This permanent state of hyper-arousal may trigger sudden mood swings.
“Mood changes may be a signal of PTSD,” says Georgia.
“That could mean becoming prone to anger, or just snapping at people and feeling quite irritable at times.”
Georgia describes how depression can also manifest as a symptom of PTSD.
“People can express that they're feeling a little bit hopeless. They might not want to go to work anymore, or their presentation could change.
“They might like to exercise, and they stop exercising. Unless they’re injured, why have they lost their motivation?”
Sleep problems
Difficulty sleeping is one of the most prevalent warning signs of PTSD, but Georgia says it isn’t always confined to nightmares.
“Nightmares and flashbacks – that experience of reliving the event – they're certainly signs of PTSD,” she says.
“But it can also be things like insomnia or not wanting to go to sleep because of that fear of what you’re going to dream about during the night.
“Sometimes people don't want to sleep in their beds anymore. They might want to sleep in a more open space like a lounge room.”
How to help
Georgia believes communication is vital for supporting a loved one with PTSD.
“The primary thing with anyone who's experiencing PTSD is, first of all, to actually listen to them,” she says.
“People are very quick to jump to conclusions about what's going on, or they might try to come up with answers like, ‘Oh, this is what you need to do’ or, ‘This is where you need to go, because so-and-so went there, and it worked for them’.”
Rather than trying to take control of the situation, Georgia recommends a gentler approach.
“By saying to them, ‘I've noticed a change in how you're behaving or what you're saying lately and I'm just wondering, is there anything going on with you?’.”
Even if the person isn’t ready to respond to you right away, Georgia says that acknowledging the issue is an important first step.
She also emphasises the importance of seeking help immediately if you suspect someone may be having a mental health crisis.
“If that person actually discloses any thoughts of harming themselves or harming somebody else – and generally it's harming themselves – because they feel quite tormented or depressed, and it seems like they're going to do that, it's really about seeking support straight away.
“That could either be through a GP, but if it's really imminent, they’re to go to hospital.”
Have hope
Thinking that your loved one may be experiencing signs of PTSD or another mental health issue can be frightening, but Georgia says it’s also an opportunity to get them help.
“For family and friends noticing differences in somebody, it's really important for them not to avoid those conversations, because avoiding them doesn't mean they're going to go away.”
She also says it’s essential to remain hopeful of a good outcome.
“PTSD is certainly treatable. It may not be curable for everyone, but some people can learn to manage their symptoms, whilst others have complete resolution of symptoms.”
If you’ve spotted the symptoms of PTSD in yourself or a loved one, support is available. Mates4Mates helps veterans and their families find a way forward by providing them with vital assistance, including psychological services. RSL Queensland also offers wellness programs to assist veterans dealing with trauma, including PTSD Resurrected and Operation PTSD Support.
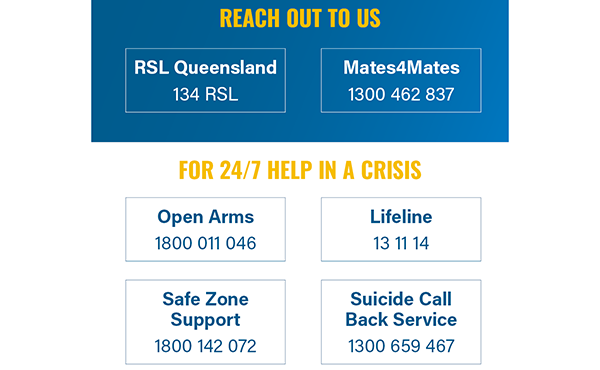
For urgent assistance, please contact any of the support services below:
The history of PTSD
p>
Related News
Loading

